What Can You Learn About Cancer Survival from a CBC?
Common Biomarkers, Cancer Progression and Survival
An excellent paper "Inflammatory markers in cancer: Potential resources * is a thorough and detailed discussion of routinely measured Cancer Biomarkers found in the inflamed tumor microenvironment that are indicative of immune capacity and prognosis. Clinicians will typically have access to a current CBC (Complete Blood Count) with differential and can readily calculate the lymphocyte ratios below
The presence of inflammatory markers is linked to both risks of cancer development and cancer survival. Cancer-related inflammation is associated with tumorigenesis and tumor progression. Increased levels of multiple biomarkers are present in the tumor microenvironment.
A thorough evaluation will include Cytokines, Leukocytes, Acute-phase proteins (ferritin, ceruloplasmin, CRP).
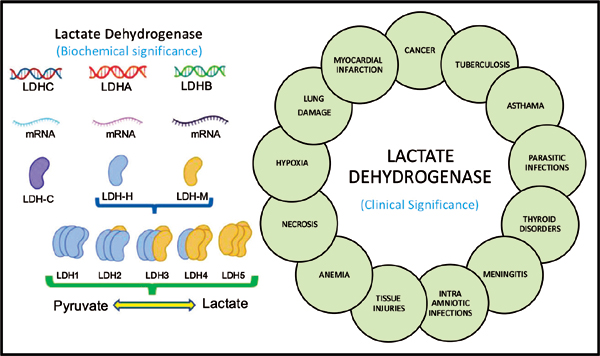
Although not routinely measured, prostaglandins, cyclooxygenases, lipoxygenases, transcription factors, and LDH may be elevated.
Cancer Related Inflammation Promotes
- Tumor Growth
- Proliferation
- Progression
- Angiogenesis
- Metastasis
- Thrombus Formation
- Immune Suppression
- Cancer Related Fatigue
- Depression
- Pain
Selected Prognostic Cancer Biomarkers from the CBC and CMP
- Neutrophil: Lymphocyte Ratio
- Lymphocyte: Monocyte Ratio
- Platelet: Lymphocyte Ratio
- CRP: Albumin Ratio
- Hypoalbuminemia
Neutrophil / Lymphocyte Ratio (NLR)
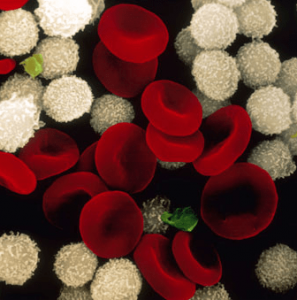 The neutrophils act as tumor-promoting leukocytes, capable of suppressing anti-tumor immune response; are effectors of angiogenesis; promote leakage of tumor cells and endothelial cells into the circulation, therefore contributing to participate in the metastatic cascade. Therefore, an elevated neutrophil count can stimulate tumor angiogenesis and contribute to disease progression, thus leading to a negative correlation between neutrophil density and patient survival.
The neutrophils act as tumor-promoting leukocytes, capable of suppressing anti-tumor immune response; are effectors of angiogenesis; promote leakage of tumor cells and endothelial cells into the circulation, therefore contributing to participate in the metastatic cascade. Therefore, an elevated neutrophil count can stimulate tumor angiogenesis and contribute to disease progression, thus leading to a negative correlation between neutrophil density and patient survival. - On the other hand, lymphocytes are a part of the host’s antitumor response the presence of lymphocytes in the tumor is associated with better responses to chemotherapy and better prognosis.
- Thus, the NLR can reflect the balance between the activation of the inflammatory pathway and the antitumor immune function.
- The division of neutrophil count by lymphocyte count is defined as NLR.
- An increase in NLR has been reported to correlate with poor prognosis in cancer patients.
- A cut-off value between 2-4 has been reported in cancer patients.
Faria, S. S., Fernandes, P. C., Silva, M. J., Lima, V. C., Fontes, W., Freitas-Junior, R., Eterovic, A. K., Forget, P. The neutrophil-to-lymphocyte ratio: a narrative review. Ecancermedicalscience, 10, 702 (2016) DOI:10.3332/ecancer.2016.702
Lymphocyte/Monocyte Ratio (LMR)
- Lymphocytopenia has been associated with increased tumor burden and poor prognosis. The probable cause could be the destruction of lymphocytes by tumor cells which decreases the body’s anti-tumor response.
- Monocytosis has also been found to be associated with poor prognosis as they Tumor-associated macrophages, which are an important mediator of cancer progression and metastases.
- The division of lymphocyte count by monocyte count is defined as LMR.
- A low LMR as a simple biomarker of the host immune system has been suggested to be related to poor prognosis in various cancers.
- The median cut-off value for LMR has been reported to be 3.0.
Nishijima TF, Muss HB, Shachar SS, Tamura K, Takamatsu Y Prognostic value of the lymphocyte-to-monocyte ratio in patients with solid tumors: a systematic review and meta-analysis. Cancer Treat Rev 41(10) 971-8 (2015) DOI: 10.1016/j.ctrv.2015.10.003
Platelet/Lymphocyte Ratio (PLR)
 Platelets are another important tumor-promoting leukocyte. They secrete vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), platelet-derived growth factor (PDGF), hepatocyte growth factor (HGF), insulin-like growth factor (IGF), transforming growth factor β (TGFβ), and many cytokines which promote epithelial to mesenchymal transition (EMT) and promote metastasis.
Platelets are another important tumor-promoting leukocyte. They secrete vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), platelet-derived growth factor (PDGF), hepatocyte growth factor (HGF), insulin-like growth factor (IGF), transforming growth factor β (TGFβ), and many cytokines which promote epithelial to mesenchymal transition (EMT) and promote metastasis. - Lymphocytes, as we know, are part of the host's defense against tumors.
- The division of platelet count by lymphocyte count is defined as PLR.
- The cutoff value estimated for PLR is 160.
- A high PLR value correlates with a poor response to therapy and a bad prognosis.
Templeton AJ, Ace O, McNamara MG, Al-Mubarak M, Vera-Badillo FE, Hermanns T, Seruga B, Ocaña A, Tannock IF, Amir E. Prognostic role of platelet to lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev 23(7) 1204–12 (2014) DOI: 10.1158/1055-9965.EPI-14-0146
CRP/Albumin Ratio (GPS_Glasgow Prognostic Score)
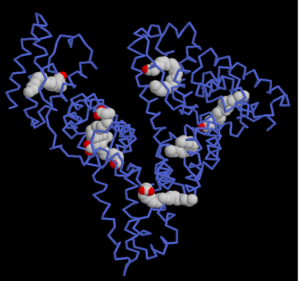 A combination of Albumin and C-reactive protein (CRP) measurements into a 3level predictive score.
A combination of Albumin and C-reactive protein (CRP) measurements into a 3level predictive score. - Patients who had both a serum elevation of CRP (>1.0 mg/dL) and hypoalbuminemia (<3.5 g/dL) were allocated a GPS of 2.
- Patients with only one of the abnormal values were allocated a GPS of 1, and
- Patients who had neither were allocated a GPS of 0.
- Survival decreases with increasing score
McMillan DC, Crozier JE, Canna K, Angerson WJ, McArdle CS. Evaluation of an inflammation-based prognostic score (GPS) in patients undergoing resection for colon and rectal cancer. Int J Colorectal Dis. 22(8):881–886 9 (2007) DOI: 10.1007/s00384-006-0259-6
Hypoalbuminemia (mGPS mGlasgow Prognostic Score)
- Patients who had both a serum elevation of CRP (>1.0 mg/dL) and hypoalbuminemia (<3.5 g/dL) were allocated a GPS of 2.
- Patients who had only serum elevation of CRP but not hypoalbuminemia were allocated an mGPS of 1, and
- Patients who had neither or only hypoalbuminemia were allocated a mGPS of 0.
- Survival decreases with increasing scores.
Similar to GPS but hypoalbuminemia = score 0
Proctor MJ, Morrison DS, Talwar D, Balmer SM, O'Reilly DS, Foulis AK, et al. An inflammation-based prognostic score (mGPS) predicts cancer survival independent of tumor site: a Glasgow Inflammation Outcome Study. Br J Cancer. 104(4):726–734 (2011) DOI: 10.1038/sj.bjc.6606087
*Richa Chauhan, Vinita Trivedi, Inflammatory markers in cancer: Potential resources
Frontiers in Bioscience, Scholar, 12, 1-24, Jan 1, 2020