Chemotherapy can lead to serious diarrhea and oral mucositis in cancer patients. This may affect the ability of a patient to complete their course of chemotherapy and to maintain proper hydration, electrolyte balance and nutritional status. Interruptions or changes to their therapeutic course of treatment may subsequently affect patient prognosis and overall survival. Skillfully managing these adverse effects is crucial to successful outcomes, nutritional status and health.
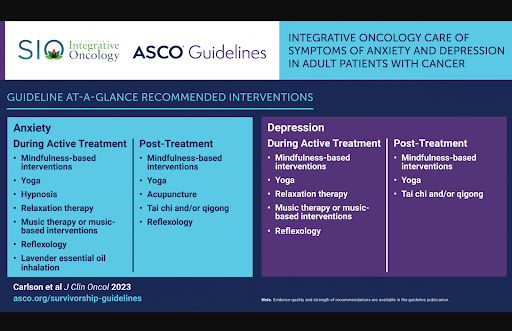
A systematic review and meta-analysis on the efficacy of oral probiotics in the management of adverse reactions to chemotherapy examined twelve trials, including 1013 patients.
An analysis of the 12 studies reviewed revealed that patients who took oral probiotics had significant decreases in diarrhea and oral mucositis.
“In contrast to the control group, orally taking probiotics significantly decreased the risk of chemotherapy-induced diarrhea (≥ 1 grade) (RR = 0.70; 95% Cl: 0.56, 0.88; P = 0.002) and oral mucositis (≥ 1 grade) (RR: 0.84; 95% Cl: 0.78, 0.91; P < 0.00001) at all grades. Further analysis found that severe diarrhea (≥ 2 grades) (RR: 0.50; 95% Cl: 0.32, 0.78; P = 0.002) and severe oral mucositis also significantly declined (≥ 3 grades) (RR: 0.66; 95% Cl: 0.55, 0.79; P < 0.00001) after oral probiotic use.”
Of note, patients taking muti-species oral probiotics had a decrease in adverse effects compared to patients taking single or dual-strain formulations.
More recent studies have also demonstrated that patients who have a healthier intestinal microbiome also have an improved therapeutic and immune response to both chemotherapy and immunotherapy treatments.
A healthy microbiome is part of our systemic immune response and systemic inflammation control.
I recommend the use of high-quality multi-strain probiotic supplements in all of my patients.
It is also important to use prebiotics simultaneously as it is the prebiotics that provide the short-chain fatty acids, the fuel of the healthy microbiota, and allow the healthy bacteria to flourish and colonize.
Prebiotics are also important to successfully supporting the intestinal microbiome. There are combination supplements that contain both probiotics and prebiotics that provide both elements.
A plant-strong diet will provide plenty of soluble fibers that are fermented in the gut and provide the short-chain fatty acids essential to a healthy and robust microbiome. These foods are excellent sources of insoluble fiber: Jerusalem artichokes, chicory, onions, leek, shallots, asparagus, beetroot, fennel, peas, cabbage, nuts and seeds and cabbage family vegetables including kale, broccoli, cauliflower, cabbage, bok choy, Brussels sprouts for example.
In contrast, insoluble fibers such as bran and cellulose found in grains and vegetables are not digested or fermented and primarily provide bulk and roughage important to intestinal tone and normal stool.)
Healthy probiotic bacteria can be found in traditional natural fermented foods from many cultures worldwide.
I recommend a teaspoon of a variety of fermented vegetables daily, such as sauerkraut, kim chi or fermented beets or carrots, for a broad spectrum of food-based probiotics. For patients who are not sensitive to dairy products, yogurt, kefir and soft goat and sheep cheese are also healthy sources of probiotics in the diet.
For patients experiencing diarrhea and mucositis, I recommend a diet of only warm, cooked food, restricting ice, cold foods and raw foods. I also recommend 2-4 cups of bone broth daily, which is rich in collagen protein and glutamine for repair as well as a good source of electrolyte replacement for a patient with diarrhea. One cup of traditionally prepared bone broth, which can be found in many natural foods stores and online, contains 10g of protein per cup. A patient drinking 4 cups daily will gain 40g of protein, important to the nutritional repletion of cancer patients who are also at risk for sarcopenia.
Probiotics, healthy commensal and symbiotic gut bacteria, and prebiotic soluble fibers from plant foods should be part of a therapeutic approach to adverse effects of chemotherapy but also part of a healthy daily diet to maintain robust microbiota in the intestines, so crucial to long-term health and wellbeing.
Selected References
Feng J, Gao M, Zhao C, Yang J, Gao H, Lu X, Ju R, Zhang X, Zhang Y. Oral Administration of Probiotics Reduces Chemotherapy-Induced Diarrhea and Oral Mucositis: A Systematic Review and Meta-Analysis. Front Nutr. 2022 Feb 28;9:823288. doi: 10.3389/fnut.2022.823288. PMID: 35299763; PMCID: PMC8922230.
Sevcikova A, Izoldova N, Stevurkova V, Kasperova B, Chovanec M, Ciernikova S, Mego M. The Impact of the Microbiome on Resistance to Cancer Treatment with Chemotherapeutic Agents and Immunotherapy. Int J Mol Sci. 2022 Jan 1;23(1):488. doi: 10.3390/ijms23010488. PMID: 35008915; PMCID: PMC8745082.
Guo C, Kong L, Xiao L, Liu K, Cui H, Xin Q, Gu X, Jiang C, Wu J. The impact of the gut microbiome on tumor immunotherapy: from mechanism to application strategies. Cell Biosci. 2023 Oct 13;13(1):188. doi: 10.1186/s13578-023-01135-y. PMID: 37828613; PMCID: PMC10571290.
Matson V, Chervin CS, Gajewski TF. Cancer and the Microbiome-Influence of the Commensal Microbiota on Cancer, Immune Responses, and Immunotherapy. Gastroenterology. 2021 Jan;160(2):600-613. doi: 10.1053/j.gastro.2020.11.041. Epub 2020 Nov 28. PMID: 33253684; PMCID: PMC8409239.